Highlights
- The No Surprises Act (NSA) protects healthcare consumers by issuing mandates that prevent surprise billing.
- Surprise billing occurs when a provider denies a claim if an insured person receives care outside the company’s network.
- NSA ensures that healthcare consumers receive affordable emergency care, eliminates balance bills for supplemental care, and requires that providers offer a clear explanation of out-of-network costs.
- NSA offers several benefits, including data transparency and increased control of healthcare spending.
- The No Surprises Act holds no surprises for Roundstone, who has always promoted data transparency.
- Members of a Roundstone group captive can benefit from increased coverage and year-over-year savings with Roundstone’s data transparency tools — the CSI Dashboard and CSI Team.
The No Surprises Act (NSA) ensures that healthcare consumers can access coverage and cost data regarding their medical care. Transparent data access is the cornerstone of excellent healthcare at affordable, predictable pricing, an outlook that group captive insurance provider Roundstone has embraced since 2005.
What is the No Surprises Act?
The No Surprises Act is part of the Consolidated Appropriations Act, signed into law on December 21, 2020, and put into effect on January 1, 2022. The NSA protects healthcare consumers from surprise billing. It achieves this by issuing mandates regarding balance billing, in-network and out-of-network provider care, and required notices about care expenses.
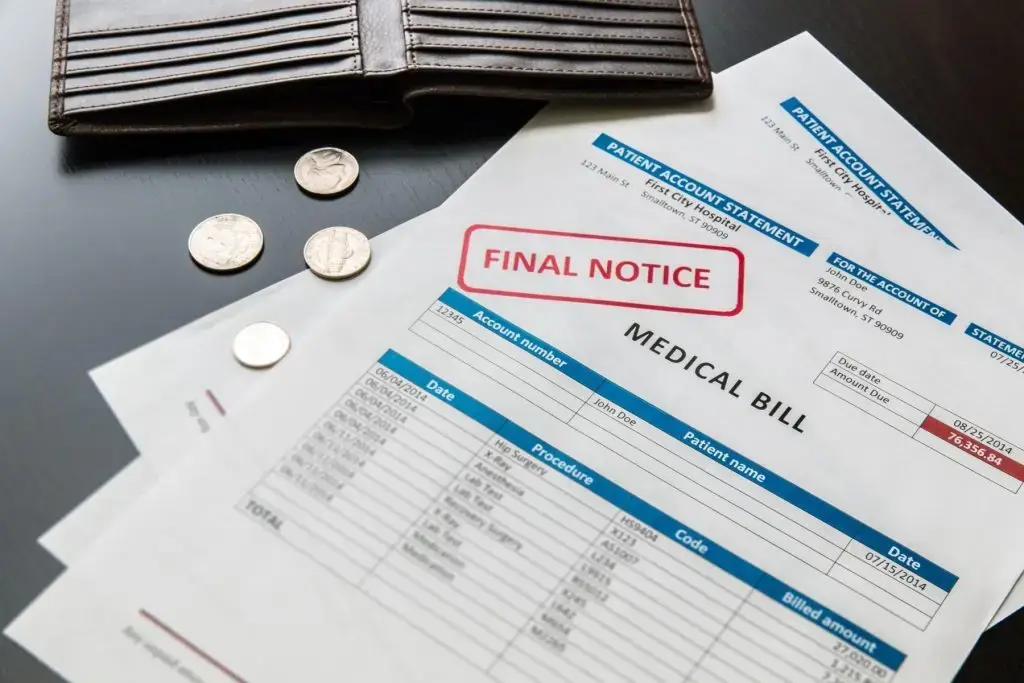
Surprise billing occurs when an insured person receives care from a provider outside the insurance company’s network. This often happens when someone receives emergency care, where they can’t choose their care provider. It also occurs with services, such as anesthesia or radiology, that don’t have an in-network option.
When this happens, the insurance company may deny the claim or only pay a portion of the medical bill, passing the remaining balance on to the consumer.
A 2020 study looked at data from over 347,356 patients and reported that 20.5% of people who had surgery at an in-network facility incurred a surprise bill. The study also found that 37% of people who received anesthesia during treatment received surprise bills, with a mean balance of $1,219.
Balance billing and unexpected out-of-network bills are forms of surprise billing, both of which the NSA aims to eliminate for healthcare consumers.

How Does the No Surprises Act Affect Healthcare Consumers?
The No Surprises Act enacts several protection measures for healthcare consumers regarding surprise billing. The No Surprises Act 2021 summary provided by the Kaiser Family Foundation (KFF) reports that the four main objectives of the act are to:
- Require insurers to cover emergency services at an in-network rate
- Ban cost-sharing by out-of-network providers for all emergency services
- Ban balance bills and out-of-network charges for supplemental care
- Require providers to provide consumers with a transparent explanation of the cost of out-of-network services
These protections offer several benefits for healthcare consumers who use private health insurance. Benefits of the new rules include more data transparency, increased control over medical care options, and fewer surprise medical expenses.
Data Transparency
The NSA embraces data transparency. It requires hospitals and healthcare facilities to provide consumers with a notice that clearly explains the costs associated with out-of-network services. The act also requires that insurance companies maintain accurate in-network provider directories and disclose broker commissions to members.
This type of data transparency allows patients to make informed decisions about their healthcare and keeps insurance companies and brokers honest.
Healthcare consumers no longer have to worry about receiving an outrageous and unexpected medical bill after obtaining medical care at an in-network facility. This allows consumers to seek appropriate care when necessary without fear of financial strain.
Increased Control
The NSA gives healthcare consumers increased control over their insurance coverage and health provider options by requiring data transparency and accountability from care providers.
Fines of up to $10,000 can result for each act of violation. This puts the power back into the patient’s hands rather than with providers and traditional health insurance carriers.
Roundstone: Embracing Data Transparency
The NSA is a significant step forward for healthcare consumers, and Roundstone applauds the move as it aligns with our core beliefs. Businesses that choose to join a group captive insurance plan from Roundstone have enjoyed claims data transparency and plan control for almost two decades.
Mike Schroeder, Roundstone CEO, explains, “Transparency to access your own data and control to impact your own costs are two of the main pillars that make a Roundstone health insurance plan really work. Transparency and control enable employers to save a significant amount of money over the long term.”
Roundstone provides tools like the CSI Dashboard and the Cost Savings Investigator (CSI) Team. These resources allow members to analyze their claims data and identify and implement cost-savings strategies.

Transparent Data Access with Roundstone
Roundstone’s group captive plans are based on the idea that your company has a right to insights from its claims data. This position differs from the traditional insurance company outlook that tends to keep you in the dark about why you are getting a rate increase year after year and what you can do about it.
CSI Dashboard
With Roundstone, you and/or your advisor can gain access to data regarding your healthcare spend through our CSI analytics dashboard. The CSI Dashboard gives you an easy-to-understand visual display of your group’s medical claims.
With the information provided by the CSI Dashboard, you can identify where you are over- or under-covered and where you can save money with a cost-containment strategy.
The CSI Dashboard lets you compare your spending to benchmark values and gives you automated monthly reports. It also explains the analytic results in an easy-to-understand format.
CSI Team
The Roundstone CSI Team is a group of individuals with varied experience in clinical care, plan document optimization, underwriting, claims, and data analytics.
When you become a group captive member with Roundstone, you are automatically assigned a CSI Team that works with your company specifically to identify and implement customized cost-saving strategies.
Our CSI Team analyzes your data on the CSI Dashboard to discover where you could benefit from cost-saving solutions. Strategies include working with a different pharmacy benefits manager, vendor, or provider. They can also help you find case management programs and institute employee well-being incentives to lower your overall healthcare costs.
Schroeder says of the CSI Team, “Roundstone’s CSI Team assumes this burden and makes regular recommendations of cost-containment programs for you, so you don’t have to spend extra time researching programs and wondering if they’re right for you. Not all insurance providers share this commitment to cost savings. It’s part of the Roundstone difference and is part of our business that we take very seriously.”
One of the best features of a Roundstone group captive plan is that once your CSI Team identifies an issue and suggests a solution, you can implement it immediately. No more waiting until renewal time; you start saving instantly with Roundstone.
Benefits of Roundstone’s Focus on Data Transparency
Although there are numerous advantages to data transparency with Roundstone’s group captive plans, the two most significant are better coverage and year-over-year savings.
Better Coverage
With the data transparency available through Roundstone’s group captive insurance plans, employers control every aspect of their coverage, ensuring they don’t pay for what they don’t need. With convenient insight into where your money is going, you can adjust your choice of providers.
We ensure you have the necessary information to make informed decisions and change course for cost containment when it suits your needs.
Year-Over-Year Savings
With Roundstone’s focus on data transparency, employers can anticipate saving a significant sum of money over the long term. You can run a cost-benefit analysis on any part of your plan at any time. This enables you to track expenses and savings so you can keep the extra cash in your bank account.
Proactive cost savings and the return of your unused premium funds result in year-over-year savings with your Roundstone plan. While you save money upfront, seeing improvements to your cash flow in just 30 days, the long-term savings are the biggest advantage of a Roundstone group captive insurance plan.
There’s no multi-year contract forcing commitment, so you can opt out at any time. However, employers who stick with the plan for at least five years see annual savings of up to 20% compared to a fully insured plan.
Avoid Surprises with Reliable Roundstone Coverage
Employers participating in Roundstone group captive insurance plans have been enjoying the same peace of mind the No Surprises Act affords since 2005.
Find out how Roundstone’s commitment to data transparency can help you find savings and take back control of your group healthcare coverage. Download your free eBook today.